In 2001, Del Bolin suffered a pulmonary embolism, a potentially deadly blood clot in his lung. During Bolin’s treatment, his doctor discovered that Bolin had a rare condition that makes him prone to blood clots. Bolin was prescribed warfarin, an anticoagulant drug with an interesting history.
Sometimes called a “blood thinner,” warfarin doesn’t actually affect the thickness of blood. Instead, the drug helps prevent the coagulation of blood, a complex cascade of biological processes the body uses to prevent an excess loss of blood from a cut or wound to the skin. However, when these coagulation processes go awry—within the veins, lungs, or brain, for example—the results can be fatal.
Now 78, Bolin lives in La Crosse and drives a disability van part time for Gundersen Health. Because he continues to take warfarin, he is less likely to develop another life-threatening clot. But he needs to be careful. Because of the way warfarin inhibits coagulation throughout his body, just a minor bump can cause bruising, and a hard blow could lead to internal bleeding. Even simple tasks, such as shaving or making dinner, are done with caution. “I’ve cut myself a couple of times over the years,” he says. “I bleed like a stuck pig.”
When Del Bolin compares himself to a bleeding farm animal, it is an apt image. The story behind the discovery of warfarin—one of the most prescribed drugs in the world—began on a farm in St. Croix County with a dead cow, a milk can full of blood, and a hundred pounds of sweet clover.
• • •
A key player in the story of warfarin is sweet clover, which grows readily in the cold climate of the upper Midwest. Brought to Colonial America from Europe in the 1600s, the bush-like Melilotus officinalis and M. alba have been used for centuries as livestock forage. Farmers in the Midwest would often harvest, dry, and store the clover to feed cattle over the winter months. However, during especially damp years the hay became contaminated with molds such as Penicillium nigricans and P. jensi. Cows fed this moldy sweet clover hay grew stiff and refused to move, often developing large bruises and blood in the urine, feces, or milk. Eventually they died from uncontrolled bleeding. The condition, common in the Midwest during the 1920s and 1930s when farmers couldn’t afford to discard moldy hay, became known as “sweet clover disease.”
On a cold Friday in 1933, at the height of the Great Depression, St. Croix County cattle farmer Ed Carlson lost two cows to sweet clover disease. He had lost three cows earlier that winter, and he knew his bull would be next, as it was bleeding from the nose. The next day, Carlson loaded a dead cow, a milk can full of its un-clottable blood, and a hundred pounds of sweet clover hay into his pickup truck and drove from his farm through a blizzard to the University of Wisconsin–Madison campus. As it was Saturday, the campus Agricultural Experiment Station was closed. After trying a few locked doors, a frustrated Carlson discovered an open door that led him to the lab of biochemist and professor Karl Paul Link.
Carlson found a sympathetic audience in Link. But the biochemist said there was little he could do but advise Carlson to throw out the spoiled hay and attempt blood transfusions on the remaining affected cows. Link later recalled how “those 190 miles of drifted roads between our laboratory and his barn must have appeared to [Carlson] like a treacherous and somber ocean.”
Link’s graduate student, Eugene Wilhelm Schoeffel, was incensed that his boss didn’t do more to help Carlson. Running his hands through the unclotted blood Carlson had left behind, Schoeffel pointed out that Carlson’s remaining cows were in danger because the farmer couldn’t afford to feed them anything but the spoiled hay. In fact, Schoeffel railed, until the problem of sweet clover disease was solved, thousands of cows across the state were in danger. “Let me tell you something,” said Schoeffel as he grabbed Link by the shoulders and demanded action, “there is a destiny that shapes our ends!” Before they closed the lab for the evening, Schoeffel had convinced Link to focus his lab’s research on the cause of sweet clover disease.

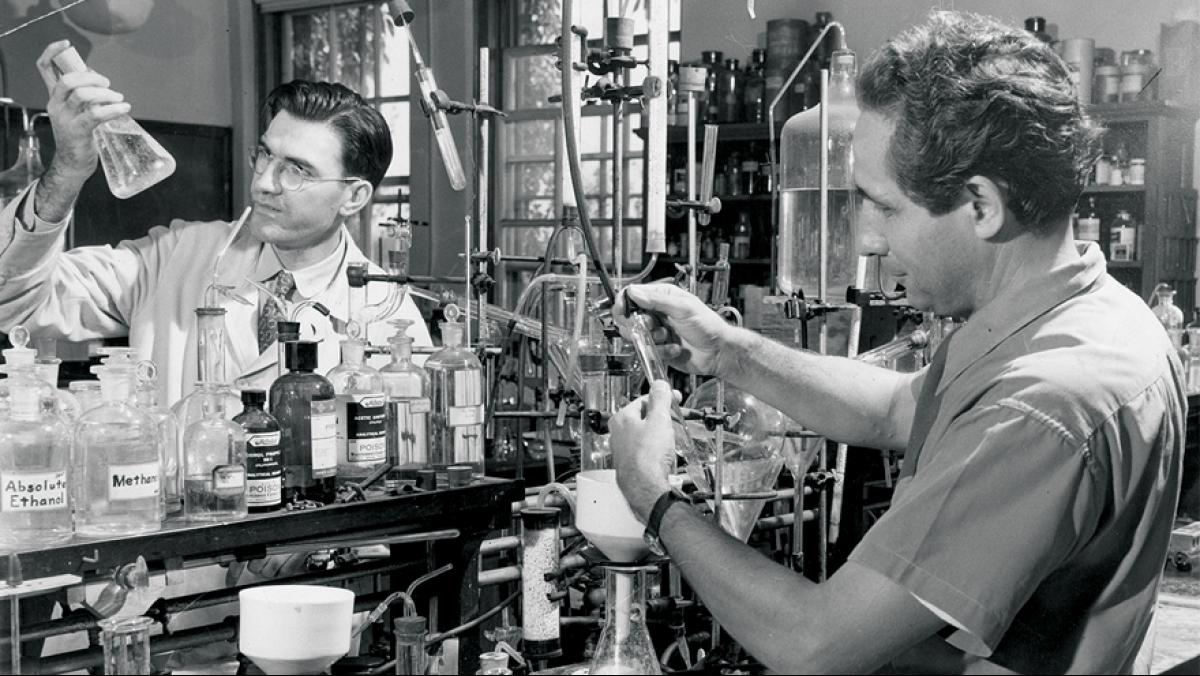
Link, along with Schoeffel and his other students, began a six-year effort to identify the hemorrhagic agent responsible for sweet clover disease. At the time, Link was already studying sweet clover, seeking a more palatable strain with low levels of a bitter compound called coumarin. Coumarin, as Link discovered, is transformed by the molds in spoiled sweet clover hay into another compound called 3,3’-methylenebis-(4-hydroxycoumarin) that reduces the level of prothrombin—an essential component for coagulation—in the bloodstream. In bringing his research interests together, Link had found the cause of sweet clover disease.
Link dubbed the newly discovered compound dicumarol, and he and his team began to synthesize more than 150 slightly different versions, testing their anticoagulant properties in laboratory rats, mice, rabbits, guinea pigs, dogs, cats, and chickens. They found that different species varied in their sensitivity to dicumarol, and that the compound affected animals differently if they were fed or fasting. Perhaps most importantly, the team discovered that dicumarol’s anticoagulant effect on the animals could be counteracted by providing them with additional vitamin K.
The role of vitamin K in the clotting process was discovered not in bleeding cows, but in bleeding chickens. Less than a decade earlier, Danish scientist Henrik Dam found that chickens fed a severely limited diet would bleed uncontrollably. Like the cows afflicted with sweet clover disease, the chickens suffered from a deficiency of prothrombin. Dam later identified the missing nutrient that could restore the clotting function and dubbed it vitamin K after Koagulation, the Danish/German word for “coagulation.”
Physician and coagulation research pioneer Armand Quick of the Marquette University School of Medicine, who had developed a laboratory assay of blood’s clotting ability, noted in 1936, “Both sweet clover disease and vitamin K deficiency emphasize the importance of prothrombin depletion as a primary cause of hemorrhage. These diseases furthermore demonstrate that the prothrombin of the blood can be diminished either by the action of a toxic substance or through the lack of an accessory food factor.” Indeed, the action of the dicumarol compounds is intimately linked to vitamin K; these compounds today are classified as vitamin K antagonists.
Thinking the dicumarol anticoagulant would have a clinical use for clotting disorders, Link patented it with the help of the Wisconsin Alumni Research Foundation (WARF) in 1941. WARF had been established in 1925 to manage professor Harry Steenbock’s patents related to vitamin D. As an independent nonprofit corporation, WARF continues to manage patents and uses the revenue to fund research at UW–Madison.
Clinical studies at the Mayo Clinic and Wisconsin General Hospital demonstrated that dicumarol was not toxic and was indeed effective at inhibiting clotting in humans. An editorial in a 1941 issue of the medical journal Lancet sang dicumarol’s praises, calling it a “rival” for heparin, the primary anticoagulant in use at the time. Dicumarol was less expensive and could be administered orally, whereas heparin needed to be given intravenously.
• • •
In 1945, after a rainy canoe trip, Link suffered a reactivation of the tuberculosis he had contracted as a student in Switzerland. He spent six months resting (and social distancing) at the Lake View Sanatorium, which is now the site of the Dane County Department of Health and Human Services. “Here I was supposed to vegetate like a topped carrot,” Link recalled. “[I] kept the aged tuberculosis out of my mind by studying laboratory records and reading the history of rodent control from ancient to modern times.” He recalled from his research how rats and mice were the most dicumarol-sensitive of all the species they had tested and decided that dicumarol—or one of its related molecules—would be an effective rat poison. He had his students re-test the compounds and found that rats were especially sensitive to compound Number 42. It was patented in 1945, again with the help of WARF, and dubbed “warfarin” in honor of both WARF and coumarin. The new compound would be, as Link called it, “a better mousetrap.”
Warfarin was marketed as a rat and mouse poison under several brand names, including d-CON. Leonard Lee Ratner, the founder of d-CON, advertised the product heavily in newspapers, over the radio, and, later, on television. Advertising was first aimed at agricultural markets, because rats caused millions of dollars in grain losses for farmers. Ratner also organized a very effective demonstration in Middleton, a Wisconsin town with a serious rat problem at the time. Beginning on November 4, 1950, d-CON rodenticide was distributed free to Middleton residents, and two weeks later there was not a rat to be found.

Warfarin was wildly successful as a rodenticide, in part because it is odorless but also because it kills slowly. An article in Sponsor magazine described how warfarin overcame the problem of bait shyness. “When other exterminators before Warfarin were tried, the clever rodents soon learned to stay away from the bait that was cutting down their numbers. … This product is so insidious that rodents never learn what is killing off their relatives.” As reported in the Peoria Heights Herald, “The rats and mice continue to eat and gradually become sleepy, walk more slowly, and finally die painlessly of internal hemorrhage.” (How the author knew the level of pain the animals perceived is a mystery.)
Since it was quite effective as a rat poison, warfarin was surely deadly for humans—at least that’s what a depressed 22-year-old army recruit thought. Determined to kill himself before being deployed to fight in the Korean War, he consumed a small amount of warfarin on March 26, 1951. Nothing happened. Still determined to kill himself, he tried again the next day. Nothing. Over the course of six days, he consumed an entire four-ounce package of the rat poison (which amounted to a hundred times the therapeutic dose). He then experienced pain in his back and abdomen, which continued to worsen until he was admitted to the U.S. Naval Hospital with vomiting, nosebleeds, and a rash over much of his body. After several blood transfusions and doses of vitamin K, the recruit physically recovered and was soon released. The physicians who treated him noted that, “Accidental [warfarin] poisoning of an adult is almost inconceivable. Taking the drug for suicidal purposes would require marked perseverance and a continued desire, lasting over several days, to die.”
The failed suicide attempt and its successful treatment with vitamin K demonstrated the relative human safety of warfarin, and further studies of the compound showed that it was more potent and faster-acting than dicumarol. Considering the reluctance of the public and medical community to associate a well-known rat poison with a human medication, a more soluble form of warfarin was licensed in 1954 with a different name: Coumadin. If there was any doubt of the efficacy or safety of Coumadin, it was surely wiped away when President Dwight D. Eisenhower began taking the drug following a heart attack in 1955.
Today, warfarin is one of the most frequently prescribed drugs in the United States. It is used to treat people with atrial fibrillation (an abnormal heart rhythm that can cause blood clots), heart valve replacements, and blood clots in the veins (deep vein thrombosis) or lungs (pulmonary embolism). It may also be prescribed to prevent blood clots and strokes after a heart attack.
• • •
As with most drugs, warfarin affects the people who take it in different ways. Factors that can influence the body’s response to warfarin include age, body weight, other medications or supplements, and diet, especially vitamin K intake. Because of this high degree of variability, patients who take warfarin must be monitored.
After open heart surgery at SSM Health St. Mary’s Hospital in Madison to repair a defective valve, Barbara Walsh was prescribed a 90-day course of warfarin. Walsh was asked to submit blood every 1 to 4 weeks during her treatment for “prothrombin time” or PT testing to measure the time it took for her blood to clot. Originally developed by Marquette University’s Dr. Armand Quick in 1935, the PT test was plagued for many years with inter-laboratory variation: identical blood samples tested in different labs could yield inconsistent results. So, in 1983 the international normalized ratio (INR) was introduced to reduce inter-laboratory variability by comparing the patient’s actual PT with a standard PT. An INR of 1.1 or less is normal for healthy individuals, while an INR of 2 to 3 is considered ideal for patients taking warfarin. (An INR below 2 may increase risk for clots, and an INR higher than 3 could lead to excessive bleeding.) Frequent testing is required to keep the INR within the narrow therapeutic range.
After submitting her blood for INR testing, Walsh would get a call from her case manager at SSM Health’s anticoagulation clinic to discuss test results and adjust the warfarin dose, if necessary. Walsh might also get advice about dietary and lifestyle changes associated with taking warfarin: avoiding alcohol and vitamin K-rich foods like spinach and kale, and being careful of falls and sharp objects.

There are more than 3,000 of these specialized clinics nationwide with highly trained pharmacists and nurses on staff who determine how often patients should check their INRs, assess patients for bleeding or clotting conditions, and adjust warfarin doses to achieve desirable INRs. Anticoagulant clinic case managers also provide guidance about changes in medication or the warfarin dosages required for dental or surgical procedures. These clinics are essential not only in helping individual patients but also in lowering the overall costs of treatment and preventing the need for emergency intervention.
In addition to the many internal and external factors that must be taken into account when treating patients with warfarin, there is yet another factor that affects dosing—genetics.
In 1961, a 73-year-old man suffered a heart attack. Afterward, he was prescribed warfarin. PT testing showed that he needed 145 mg of warfarin per day to achieve the desired anti-clotting effect, a nearly twenty-fold increase over the average dose. Coincidentally, and unknown to him at the time, his identical twin brother suffered a heart attack the same week. The twin also showed an unusual resistance to warfarin, as did several other (but not all) family members. Clearly, warfarin resistance is hereditary. The authors of the paper in the New England Journal of Medicine documenting the case proposed that the trait was due to alteration of a protein involved in the vitamin K-dependent production of clotting factors. But they didn’t know which of the thirteen distinct proteins involved in the multiple steps of coagulation were altered.
At around the same time, some wild rats and mice developed resistance to the lethal effects of warfarin. Link and his UW–Madison colleagues Mark A. Hermodson and John W. Suttie (who later elucidated the molecular function of vitamin K) obtained descendants of some resistant wild rats from Wales. They reached a conclusion similar to that of the researchers studying human resistance to warfarin: that a mutation altered a protein needed for production of clotting factors, making that protein less able to bind to warfarin and thus less able to be inhibited by it. While the altered protein was finally identified in these rats by researchers Alicia Zimmermann and John T. Matschiner at the University of Nebraska College of Medicine in 1973, it wasn’t until thirty years later that the gene and mutations that confer warfarin resistance were identified.
The genetic variation described in resistant people and rats affects a protein called Vitamin K epoxide reductase complex 1 (VKORC1) that makes vitamin K available to help produce clotting factors. Normally, warfarin blocks its action, depleting levels of vitamin K and reducing clotting ability. Warfarin binds poorly to the altered protein, however, and higher doses of warfarin are needed to achieve ideal INR levels in people with VKORC1 variations.
Another protein affecting warfarin dosing is Cytochrome P450 2C9 (CYP2C9). Altered forms of this protein are less effective at metabolizing warfarin, a so the drug accumulates in the body. People with this genetic variation need lower doses of warfarin to keep their INR levels in the therapeutic range.
In 2010, the FDA recommended that patients be tested for the mutated proteins VKORC1 and CYP2C9 before starting on warfarin so the initial dose would be more likely to have the desired effect on INR. Although genetic testing has become cheaper and easier, it is not commonly used for warfarin dosing in Wisconsin due to the limited availability of timely testing. Even so, a study published in 2019 by Marshfield Clinic examined an existing database of genetic information from 749 patients and found it took less time for patients to reach a stable INR when these genetic variations were taken into account.
Scott Hebbring, a Research Scientist at Marshfield Clinic, points out that the use of genetic information to inform dosing would be especially useful for patients in rural areas who currently “need to travel an hour or two a day to get their INR taken, just to get them on their proper dose.”
• • •
In 2010, the FDA approved the first new anticoagulants in more than fifty years. Called direct oral anticoagulants (DOACs), these drugs—dabigatran, rivaroxaban, apixaban, edoxaban, and betrixaban—act on specific factors in the clotting cascade and are unaffected by vitamin K. In general, DOACs have a quicker anticoagulant effect than warfarin and are cleared from the body sooner. A major advantage of DOACs over warfarin is that they do not require frequent INR monitoring.
While studies comparing the effectiveness of warfarin and DOACs in various populations are ongoing, DOACs were added to the National Patient Safety Goal for anticoagulant therapy in summer 2019. “About half of the patients that were on warfarin have switched over to DOACs,” says Anne Rose, PharmD, who manages UW Health’s anticoagulation clinic. “DOACs are now the preferred treatment for patients with atrial fibrillation, an abnormal heart rhythm that can produce clots. Warfarin, however, is more effective than DOACs in patients with heart valve replacements.”
 Even with the advent of the lower-maintenance DOACs, anticoagulation clinics continue to be a vital resource, especially in light of new research that shows blood clots play a role in COVID-19. The new information makes the management of anticoagulants even more complicated. “That’s where we struggle,” says Rose. “We know that there is a tendency towards [COVID-19] patients having more blood clots. We are not really sure why. … Right now the big discussion is ‘How do you prevent those things from happening?’ ”
Even with the advent of the lower-maintenance DOACs, anticoagulation clinics continue to be a vital resource, especially in light of new research that shows blood clots play a role in COVID-19. The new information makes the management of anticoagulants even more complicated. “That’s where we struggle,” says Rose. “We know that there is a tendency towards [COVID-19] patients having more blood clots. We are not really sure why. … Right now the big discussion is ‘How do you prevent those things from happening?’ ”
The challenge of preventing dangerous blood clots will go on, and warfarin will continue to play a key role. “There is still a place for warfarin,” notes Rose, “and I think there will always be a place for it.”
Warfarin has had a circuitous history, progressing from a feed contaminant to a rat poison to an important anticoagulant. No one appreciated the ins and outs of this story more than Karl Paul Link, who always enjoyed a colorful retelling of it in print and in lectures. Although Link is credited with warfarin’s discovery, he did acknowledge his students’ contributions. Many of them were war veterans, young men who “never ceased to wonder [and] kept on trying,” recalled Link. “They were on a project directed toward doing mankind some good instead of trying to destroy it.”
Although Link and his students couldn’t save Ed Carlson’s cows, through the discovery of warfarin they truly did do mankind some good.